The “Hospitals as Insurers” Trend: Marketing Implications and Opportunities

The Affordable Care Act (ACA) isn’t just changing healthcare models from the consumer perspective, but for providers and insurers, as well. And as healthcare reform takes hold (look at exchanges in the states of New York,Vermont and Massachusetts) and as healthcare systems feel increasing pressure to be accountable for patient care, look for major developments in the marketplace. One that’s well on its way? Hospitals as insurers.
We should expect more and more headlines like this one: “North Shore-LIJ Health System to Launch a Health Plan.” In fact, a healthcare economist in that article notes a “growing trend towards payer-provider integration,” and a recent survey by a Washington, D.C. research firm predicts one in five health systems to become payers by 2018.
The trend
In the traditional “fee-for-service” model, consumers (often along with their employers) fund premiums, co-pays and other forms of coinsurance. When a patient receives care, the provider bills the insurance company. Prices are pre-determined (negotiated as part of contracts between providers and insurers), and no money is paid until a triggering event, like a visit to the doctor or a procedure at a hospital.
Newer models push providers toward more “accountable care.” For example, insurance company may refuse to reimburse when a patient needs to be readmitted within a certain timeframe following a procedure or treatment. And in another variation, insurance companies may pay health systems a flat monthly rate per member for providing all necessary care.
What happens with increased emphasis on provider accountability (translation: health systems are on the hook more and more for the cost of care) is that hospitals are saying, “If we’re accountable anyway, why not do it ourselves?”
As insurers, hospitals believe they can be competitive for a number of reasons, including anticipated savings, such as lower administrative costs. In the North Shore-LIJ example above, its hospital-based health plan is priced lower than other plans in its area.
Critics of hospitals as insurers worry it’s a case of the fox guarding the hen house. Can – and will – hospitals be fair? Will they value second opinions? What about procedures patients seek outside the health system… if, for example, another provider has greater expertise?
Marketing implications and opportunities
To say the least, all of this creates an interesting marketplace. For one thing, hospitals may now be competing alongside the same insurance companies from whom they continue to receive revenue. And for another, as exchanges make some first apples-to-apples comparisons and put cost at the forefront, transparency will become a requirement.
A great example of this can be found on the state healthcare exchange websites. The homepage for Vermont’s exchange leads with this: “Make side-by-side comparisons of health plans.”

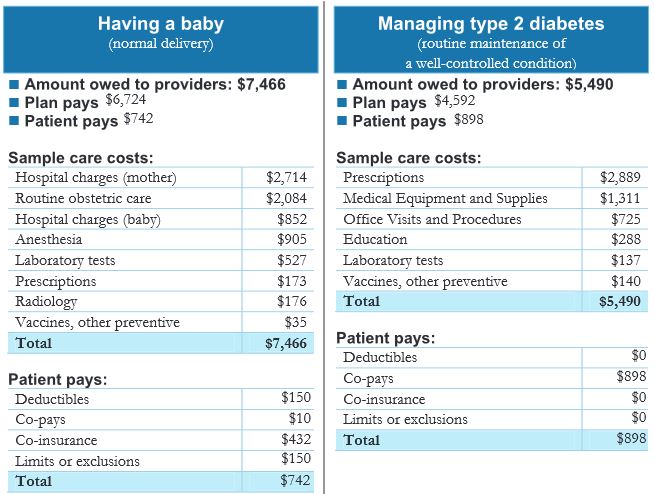
Deeper into the site, users can review summaries of benefits and coverage, which show detailed costs for having a baby and managing type 2 diabetes. This kind of information (see screenshot below) has never been seen by most consumers and is likely to raise new questions when they shop for such services.
Despite the frenzy big changes like the ACA can cause, now is an excellent time to be in the healthcare marketplace: consumer buzz and attention around healthcare have never been this intense… at least not in the three decades Media Logic’s been doing this work. Health systems and insurance companies have a curious and interested audience, not only on the national stage but also at the individual level where purchasing decisions are made. Being in the mix now, providers and insurers – along with the new payer/provider hybrid – have great opportunities to capture new business.
And so as we keep an eye on this as it evolves, we’re curious: What challenges and opportunities do you foresee?






