Improve Your ROI on Telemedicine Through Better Employee Communications

While only a minority of U.S. employers offered telemedicine as an employee benefit five years ago, today, approximately 70% of large employers offer it, based on findings of a survey by the National Business Group on Health. Despite the impressive increase in adoption of telemedicine coverage, the study also revealed that only 3% of employees offered the service actually made use of it, falling far short of the ideal minimum of a 30% utilization rate. This means delayed ROI on cost, time and productivity to payers, providers, employers and employees.
This gap in utilization is widely attributed to a lack of education among employees on how and when to access telemedicine services. Employers must realize that making the switch from doctor or urgent care office visits to engagement with telemedicine requires a combination of top-of-mind awareness, comfort level and perceived value over habitual behavior on the part of their employees. Employers can help close the gap with a smart communications approach that relies on appropriate channels and the right messaging.
Employers can promote utilization through communications that include employee handouts, breakroom and bathroom posters, refrigerator magnets, payroll stuffers, newsletter content, email reminders, social channels and video demos. They can also facilitate utilization by providing a private kiosk or office space where employees can access telemedicine providers. HealthPerx, a health and lifestyle benefits program that features telemedicine as its core benefit, sees improvement to a 25-60% utilization rate upon its clients’ implementation of its monthly flyer and video content to businesses and employees. Naturally, employer and payer implementation of a communications program should be tailored to how best to connect with specific employee groups. For example, if there are language needs required, be sure to communicate multi-lingual availability. Likewise, email may not be best for employees on the manufacturing line, whereas it would be ideal for companies with office-based and heavy travel staffs.
Content should explain how telemedicine services work, not as a replacement for their primary care, but as a convenient, competent, cost and time-saving complement. Employees should be educated on what symptoms and conditions are ideal for initial telemedicine consultation, how to engage the service, what to expect of the experience and what the cost will be. Making the first visit free can help to drive trial and, ultimately, adoption. Associating reminders with seasonal symptoms can be a great way to keep the service top of mind for trial.
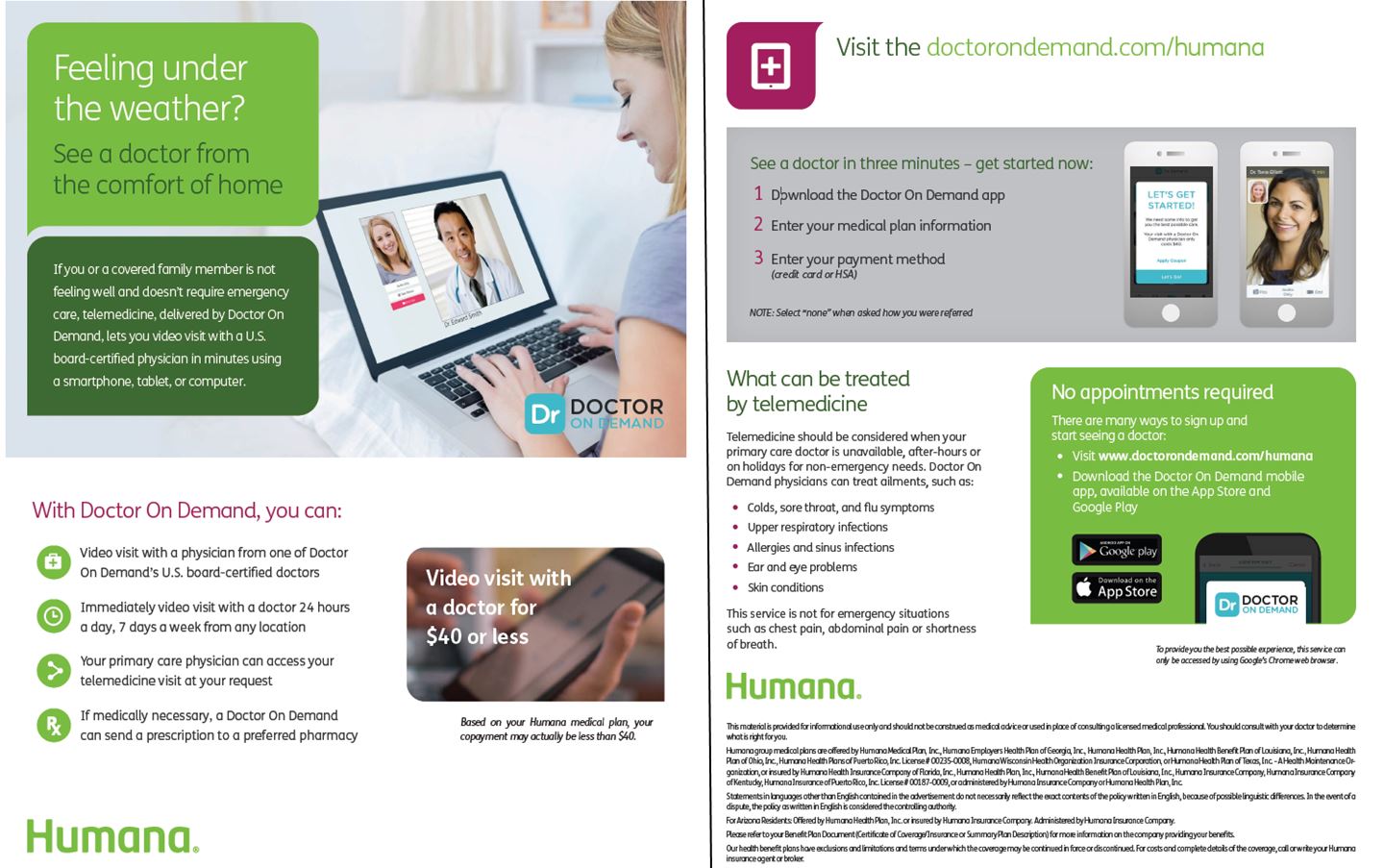
A number of telemedicine providers such as American Well, Teladoc, First Stop Health and Doctor on Demand provide welcome kits and other marketing materials that insurers and employers may use to facilitate employee utilization. If the telemedicine provider hasn’t supplied materials for all required channels, employers may request the telemedicine provider develop additional components as part of the contract and/or the employer or insurer may need to fill the gap. The key is to implement any and all of the available communication resources for each workforce, or create others as needed. Using multi-pronged communication from both employers and health insurers, rather than unilateral communications, will more strongly position telemedicine as a top-of-mind resource.
Here are some samples of how Humana implemented co-branded components of Doctor on Demand’s marketing kit.
By 2019, somewhere between 90 and 97% of employers are expected to be offering telemedicine. However, with large investments and expectations for ROI on the line, employees may need to “use it or lose it.” Investing stakeholders will only sustain the benefit for so long before abandonment. Employee communications are a relatively easy way to move the needle on adoption on a significant scale. Assuming quality of service and positive outcomes, old fashioned word of mouth and promotion of referral to colleagues and covered family members will help drive forward momentum.









